To improve uptake and yields in index testing, five facilities in Kigali were selected as pilot sites for intensive CQI. The Ciheb team, in conjunction with the Centers for Disease Control and Prevention, conducted site visits to identify on-site challenges to service uptake and assess capacity of health facilities to implement CQI. These facilities were supported to develop a functional quality improvement team that would identify gaps and implement CQI projects. The CQI team included the director of the health facility, ART clinic supervisor, ART nurses, VCT, PMTCT and ANC focal persons, social worker, data manager, and district nurse mentor. The CQI teams were trained on how to implement and sustain CQI activities, including structured root cause analysis and developing “change packages,” using a priority matrix to identify solutions, and using data to measure progress. After initial training and continuous mentorship, the CQI teams developed CQI projects to respond to identified gaps across the index testing.
Index testing, also known as partner notification, is an effective case-finding strategy that targets the exposed contacts of HIV-positive persons for HIV-testing services. It is a voluntary process where counselors and/or healthcare workers ask index clients to list all of their sexual or injecting drug partners within the past year and their children.
The index testing cascade is as follows:
- Number of eligible people living with HIV (PLHIV) offered index services
- Proportion of index cases who accepted index testing service
- Number of index case partners contacted and tested for HIV
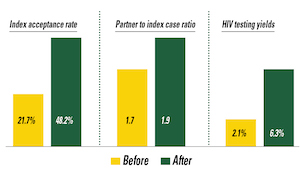 The CQI team revised their change packages and adjusted work plans and indicator targets. Mentorship and support continued through phone calls. Intensive site-level monitoring and mentorship combined with improved CQI capacity at the site level led to improved index testing performance. The index acceptance rate increased from 21.7% to 48.2%, partner to index case ratio increased from 1.7 to 1.9, and HIV testing yields increased from 2.1% to 6.3%. Qualified and trained HIV counselors and dedicated index testing services staff were key towards the best practices. The next step includes scale-up of this CQI model to the remaining 18 Kigali sites and providing continuous mentorships, on-the-job trainings, and holding regular data reviews, peer learning, and experience sharing.
The CQI team revised their change packages and adjusted work plans and indicator targets. Mentorship and support continued through phone calls. Intensive site-level monitoring and mentorship combined with improved CQI capacity at the site level led to improved index testing performance. The index acceptance rate increased from 21.7% to 48.2%, partner to index case ratio increased from 1.7 to 1.9, and HIV testing yields increased from 2.1% to 6.3%. Qualified and trained HIV counselors and dedicated index testing services staff were key towards the best practices. The next step includes scale-up of this CQI model to the remaining 18 Kigali sites and providing continuous mentorships, on-the-job trainings, and holding regular data reviews, peer learning, and experience sharing.
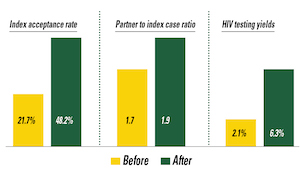 The CQI team revised their change packages and adjusted work plans and indicator targets. Mentorship and support continued through phone calls. Intensive site-level monitoring and mentorship combined with improved CQI capacity at the site level led to improved index testing performance. The index acceptance rate increased from 21.7% to 48.2%, partner to index case ratio increased from 1.7 to 1.9, and HIV testing yields increased from 2.1% to 6.3%. Qualified and trained HIV counselors and dedicated index testing services staff were key towards the best practices. The next step includes scale-up of this CQI model to the remaining 18 Kigali sites and providing continuous mentorships, on-the-job trainings, and holding regular data reviews, peer learning, and experience sharing.
The CQI team revised their change packages and adjusted work plans and indicator targets. Mentorship and support continued through phone calls. Intensive site-level monitoring and mentorship combined with improved CQI capacity at the site level led to improved index testing performance. The index acceptance rate increased from 21.7% to 48.2%, partner to index case ratio increased from 1.7 to 1.9, and HIV testing yields increased from 2.1% to 6.3%. Qualified and trained HIV counselors and dedicated index testing services staff were key towards the best practices. The next step includes scale-up of this CQI model to the remaining 18 Kigali sites and providing continuous mentorships, on-the-job trainings, and holding regular data reviews, peer learning, and experience sharing.

